You are here: Home: CCU 4 | 2005: Lee
M Ellis, MD
| Lee M Ellis, MD |
EDITED
COMMENTS |
 Potential
mechanism of action of anti-VEGF therapy Potential
mechanism of action of anti-VEGF therapy
Now that bevacizumab is approved as front-line therapy for
colorectal cancer in combination with intravenous 5-FU, ongoing
laboratory experiments are attempting to determine its mechanism
of action. Most believe it is anti-angiogenic; however, recent
papers from Harvard and Massachusetts General Hospital have
shown that anti-VEGF therapy can normalize the tumor vasculature.
Normal vasculature is efficient, whereas abnormal tumor
vasculature is inefficient. Rakesh Jain demonstrated that
approximately five days after anti-VEGF therapy was administered
to a mouse, abnormal tumor vasculature became more normalized
(Winkler 2004). From a laboratory perspective, I believe
a biphasic response occurs with anti-VEGF therapy. Initially,
it may help the delivery of chemotherapy, and in the long
term it may be truly anti-angiogenic.
Jain has hypothesized that an early window of opportunity
exists for enhancing the uptake of chemotherapy or oxygen
for radiation therapy. One of the advantages of bevacizumab
is that it has a long half-life. After administering one
dose of bevacizumab, the half-life is approximately 20 days,
so if bevacizumab is combined with intravenous 5-FU, FOLFOX,
FOLFIRI or other agents, we’re likely to hit that window
of opportunity, resulting in true enhancement of the effects
of chemotherapy.
Bevacizumab in combination therapy
At ASCO 2004, it was reported that bevacizumab improved
the efficacy of 5-FU/leucovorin in patients with first-line
metastatic colorectal cancer who were not ideal candidates
to receive irinotecan (Kabbinavar 2004, 2005a, 2005b). The
study did not reach its primary endpoint in overall survival
because too few patients were enrolled; however, approximately
a four-month improvement in overall and progression-free
survival was seen, which was statistically significant and
similar to that seen in other trials.
Giantonio presented data demonstrating that bevacizumab
improved the efficacy of FOLFOX (Giantonio 2005a, 2005b).
Clinical trials have also shown that anti-VEGF therapy — bevacizumab
being the most studied — also improves the effects
of IFL (Hurwitz 2004). We assume it would also improve the
efficacy of FOLFIRI. Since we aren’t sure of the mechanism
of action of anti-VEGF therapy, we don’t know whether
bevacizumab would be better with one agent versus another.
One interesting study reported at the ASCO GI meeting this
year is BOND-2, which is a randomized Phase II trial of cetuximab/bevacizumab/irinotecan
versus cetuximab/bevacizumab in irinotecan-refractory colorectal
cancer (Saltz 2005a, 2005b). It will be interesting to see
whether bevacizumab can improve the effects of cetuximab — two
biologic agents — without any chemotherapy in the second-line
setting.
Combination of anti-VEGF therapy with
chemotherapy to enhance the effects of radiation therapy
in the neoadjuvant rectal cancer setting
To most patients, sphincter preservation is extremely important.
Many patients will accept a therapy with a higher risk of
recurrence in order to maintain sphincter function and avoid
a colostomy. In residency, I learned that life with a colostomy
is greatly overrated. Patients will travel far and consult
with numerous surgeons in order to find one who will try
to save their sphincter. Unfortunately, if a tumor clearly
involves the sphincter, little can be done to save the sphincter
mechanism.
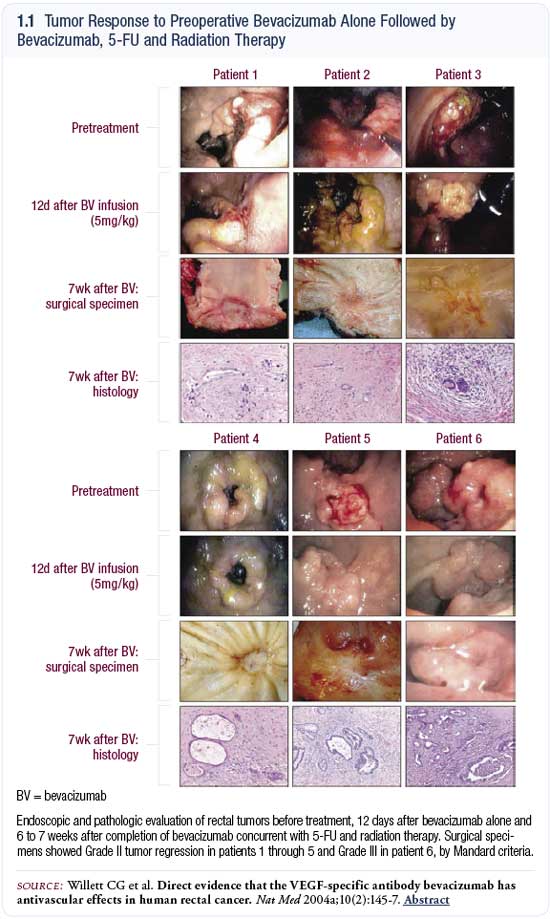
For these reasons, the advent of neoadjuvant chemoradiation
therapy followed by sphincter preservation surgery is critically
important. In a clinical trial conducted by Willett at Massachusetts
General Hospital, bevacizumab was used with 5-FU to enhance
the effects of radiation therapy preoperatively (Willett
2004a). In 2004, Willett published in Nature Medicine photos
of the responses that were obtained with this novel regimen
(1.1, 1.2; pages 8-9). All six patients had a near-complete
response, and there was just a little ulcer remaining where
the tumor was before.
The concept of adding bevacizumab is being expanded upon
by Willett and other institutions, such as MD Anderson and
Sloan-Kettering. At ASCO in 2004, Willett presented follow-up
data with approximately 11 patients, and they all appear
to have a better gross clinical response than we would expect
with only microscopic patches of tumor cells remaining (Willett
2004b).
The overall analysis hasn’t been done, and this is
a very small number of patients. However, we should follow
this in the future and see if with a larger number of patients
we continue to observe this excellent pathologic response
to the combination of anti-VEGF therapy, chemotherapy and
radiation therapy.

Laparoscopically assisted versus open colectomy
Laparoscopic surgery is safe when performed by an experienced
surgeon. From a patient’s perspective, it is critical
to use a surgeon who has been trained in this technique or
has performed at least 50 cases. Many of us in academic centers
don’t typically see patients with early-stage tumors,
and for that reason have fewer patients undergoing laparoscopically
assisted colectomy than in community practices.
Laparoscopically assisted colectomy has taught us that
we can remove the colon through a smaller incision, and we
believe patients recover better with smaller incisions. When
performing an open colectomy, we now make smaller incisions
and use retractors more efficiently. However, a study published
in the New England Journal of Medicine, which randomly
assigned patients to laparoscopically assisted versus open
colectomy, reported a surprising variability in the length
of incisions in both groups, ranging from two or three centimeters,
respectively, to 35 centimeters (Clinical Outcomes of Surgical
Therapy Study Group 2004).
While I believe the open technique is safer, I respect
the opinions of the physicians who are experts in laparoscopic
surgery. Laparoscopically assisted colectomy is preferable
in some cases, such as in an elderly patient with a poor
performance status who has a small tumor in the sigmoid colon
or right colon. The laparoscopic surgery requires more time
in the operating room, but an experienced surgeon can perform
these cases relatively quickly.
I am more comfortable with the open technique because it
allows me to palpate around the abdomen. We can do a laparoscopic
ultrasound of the liver and run the bowel, but to me, nothing
compares to that tactile sensation. Sometimes I can feel
a lymph node at the base of the mesentery that can’t
be seen, or I feel things on the liver that I may not see
with a laparoscope. Tactile sensation is important to get
a good feel for the location of the tumor, the lymph nodes
and anything else that may be going on in the abdomen.
Select publications
 |
| Dr Ellis is a Professor of Surgery and
Cancer Biology at The University of Texas MD Anderson
Cancer Center in Houston, Texas. |
|

