| Tracks 1-14 |
| Track 1 |
Introduction |
| Track 2 |
OPTIMOX2: Maintenance therapy
versus chemotherapy-free
intervals |
| Track 3 |
Selection of patients with
metastatic disease for an
intermittent chemotherapeutic
strategy |
| Track 4 |
Determination of bevacizumab
dose in combination with
chemotherapy |
| Track 5 |
Societal and economic impact of
the cost of cancer therapies |
| Track 6 |
Predictors of response to EGFR
and VEGF inhibitors |
| Track 7 |
Key clinical research questions
regarding the use of biologic
therapies |
|
| Track 8 |
Use of cetuximab/bevacizumab
combination antibody therapy |
| Track 9 |
Clinical trials evaluating curative
intent strategies for patients with
initially unresectable metastatic
disease |
| Track 10 |
Geographic differences in the
tolerability of capecitabine |
| Track 11 |
Intensive surveillance for early
identification of metastatic
disease after adjuvant therapy |
| Track 12 |
Changing patterns of metastases
in colorectal cancer |
| Track 13 |
Selection of adjuvant therapy for
elderly patients |
| Track 14 |
Selection of an oral versus
intravenous fluoropyrimidine as
monotherapy |
|
|
Select Excerpts from the Interview
Track 4
 DR LOVE:
DR LOVE: What are some of the common issues raised to you by
oncologists in practice?
 DR MEROPOL: One of the questions that has recently been raised is, “What
is the appropriate dose of bevacizumab to use with chemotherapy for patients
with colon cancer?” The original FDA-approved dose was 5 mg/kg every two
weeks, based on the IFL data (Hurwitz 2004).
DR MEROPOL: One of the questions that has recently been raised is, “What
is the appropriate dose of bevacizumab to use with chemotherapy for patients
with colon cancer?” The original FDA-approved dose was 5 mg/kg every two
weeks, based on the IFL data (Hurwitz 2004).
ECOG-E3200, a study for patients who had not previously received bevacizumab
but had failed prior therapy with 5-FU and irinotecan, demonstrated
a survival advantage with the administration of FOLFOX and bevacizumab.
It is interesting that the dose of bevacizumab in ECOG-E3200 was 10 mg/kg every two weeks (Giantonio 2005).
On the one hand, we have IFL with bevacizumab at 5 mg/kg demonstrating
a survival benefit (Hurwitz 2004). Of course, IFL is a chemotherapy regimen
we don’t use much anymore. I believe most of us who treat many patients with
colon cancer are comfortable with 5 mg/kg regardless of the regimen.
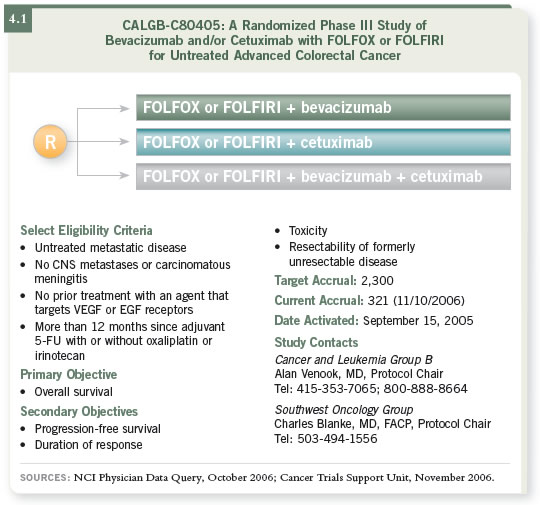
More data will be forthcoming from the current Intergroup study (C80405),
in which patients will receive chemotherapy (FOLFOX or FOLFIRI) with
bevacizumab, cetuximab or the combination as front-line therapy (4.1). This
study uses a 5-mg/kg dose of bevacizumab. So we will have additional information
about FOLFOX with 5 mg/kg of bevacizumab.
Track 7
 DR LOVE:
DR LOVE: What do you think are the most exciting clinical research
questions being asked in the current trials?
 DR MEROPOL: One of the key questions is whether one should continue
bevacizumab after the failure of a front-line regimen containing bevacizumab.
DR MEROPOL: One of the key questions is whether one should continue
bevacizumab after the failure of a front-line regimen containing bevacizumab.
That is, perhaps, the most important clinical question we have in the treatment
of metastatic disease.
Studies are in development that we hope will answer this question. One study
will randomly assign patients who experience disease progression on a frontline
bevacizumab-containing regimen to continue or not continue bevacizumab
with their next line of therapy. At this point, I am not continuing
bevacizumab with second-line therapy.
Another important question in clinical trials is whether combinations of VEGF
and EGFR antibodies as front-line therapy will provide better outcomes in
progression-free or overall survival. The question is being evaluated both
with cetuximab and panitumumab. A third key clinical question relates to the
adjuvant setting. Studies are under way exploring whether bevacizumab or
cetuximab should be used in the adjuvant setting. That is incredibly important.
Also, some large-scale studies are exploring whether treatment can be assigned
on the basis of molecular markers in the tumors. Two studies at the cooperative
group level are taking this approach. In ECOG-E5202, an adjuvant trial
for patients with Stage II colon cancer, the markers being used are microsatellite
instability and loss of heterozygosity at chromosome 18q. Based on these
markers, a decision is made about whether the patient can be safely observed
or whether he or she should receive chemotherapy.
In the metastatic disease study ECOG-E4203, the marker being evaluated is
thymidylate synthase (TS). The hypothesis is that if your tumor has a high
level of TS, you are more likely to be resistant to 5-f luorouracil. Patients
whose tumors have high TS levels, measured by immunohistochemistry, are
randomly assigned to FOLFOX/bevacizumab or a non-5-FU-containing
regimen (irinotecan/oxaliplatin/bevacizumab). Those whose tumors have a
low to intermediate TS level are assigned to FOLFOX/bevacizumab.
Select publications

